- 0 replies
- 264 views
- Add Reply
- 0 replies
- 423 views
- Add Reply
- 0 replies
- 1,427 views
- Add Reply
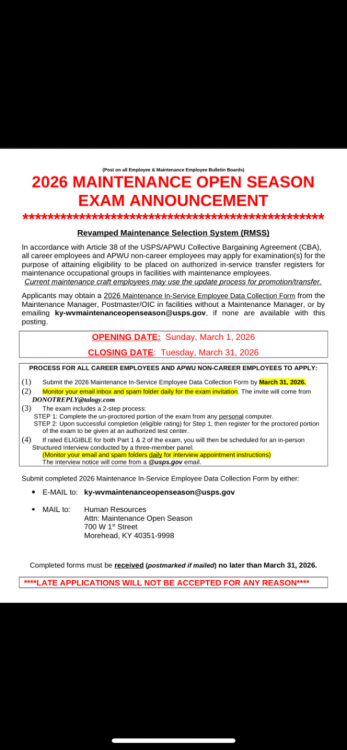
Maintenance Open Season
2026 Pay Period Calendar and Leave Chart Available
By Apwu133,
Clerk Division Settles Three Major Postal Support Employee National Disputes
By Apwu133,
November meeting notice
New health plan places for 2026
By Apwu133,