All Activity
- Earlier
-
The attendeies at the 2024 National Convention who spoke and voted on many issues that effect all APWU 133 members.
-
POSTAL SERVICE HEALTH BENEFITS (PSHB): This is Kayla “Cuppy” Reynolds, your APWU Health Plan Representative and Tour 1 Steward, with some information about the changes coming to the health plans in 2025. Currently both the APWU Consumer Driven Option (CDO) and High Option (HO) have been conditionally approved based on benefits and rate negotiation over the summer. This negotiation normally takes place every summer and we should know what the rates and benefits will be in October of 2024. Rates and benefits change a little nearly every year. Normally the APWU Health Plan will have this information before the Open Season Seminar, which is occurring October 16 – 20, 2024. Current plan benefits and information are available at apwuhp.com All of the Health Plans currently available to Postal Service Employees will be going through this process, and the enrollment codes will be changing. Currently if you go to OPM.gov you can look at what plans should be available during open enrollment. To do this, you need to go to the “insurance” heading and select the “FEHB Plan Comparison Tool” and after inputting your zip code select “Federal & U. S. Postal Service (USPS) Employee “. Keep in mind that the rates you will see displayed are for the current year, NOT for 2025. Those rates are renegotiated every year, for all plans, not just the APWU health plans. Remember that the Union has currently negotiated for the USPS to pay 95% of the premium costs for the APWU CDO and that the premiums listed would be for non-union members, Postal Support Employees, or newly Career employees who have not had a Federal Employee Health Benefit plan for 1 year yet. This is the ONLY Health Plan that offers that type of reduction, and is one of your many benefits of being an APWU member. For instance, a career employee who paying for the Self Only APWU CDO plan pays only $15.36 in a premiums, whereas a non-member would pay $76.78. That is a difference of $61.42 each pay period, which over the course of the month, is nearly four times what they would pay in Union dues! Union dues for our local for a career employee are currently $34.11 per pay period. As a reminder, the USPS Health Benefit Plan for Postal Support Employees is NOT a Federal Employee Health Plan. PSEs are eligible to enroll in the APWU CDO after one year of employment with the Postal Service. In their first year of employment they are only eligible for the USPS plan, currently administrated by BlueCross BlueShield. Once they hit one year, they are only eligible for either that plan, or the APWU CDO plan. Once career, they no longer qualify for the USPS Health Benefit Plan and MUST choose one of the other Health Plansavailable to career employees, otherwise they will lose coverage 30 days after being converted. For Retirees or those with questions about Medicare, please check keepingposted.org for helpful links, articles and online recordings. You can also find contact information for retirees. Open Season will occur November 11 – December 9, 2024, and Health Nurse Kelley Moore has confirmed that local Health Fairs will be occurring November 4 – 8, 2024. As more information is made available to us, we will be sure to keep the membership updated!
-
Opening Day Comments – National Negotiations -- June 25, 2024 By APWU President and Lead Negotiator Mark Dimondstein The American Postal Workers Union, AFL-CIO welcomes this opportunity to represent approximately 200,000 postal workers in these important negotiations for a new Collective Bargaining Agreement between our union and the United States Postal Service. For generations postal workers were denied our right to negotiate over wages, benefits, and conditions of employment. Instead, workers were compelled to engage in what we called “collective begging” to Congress -- and our livelihoods were subject to the whims of politicians and political parties. That changed 54 years ago, when postal workers won true collective bargaining rights resulting from the Great Postal Strike of 1970. Since that historic strike, postal workers’ lives have vastly improved. Now representatives of our union sit across the bargaining table from management as equals – not because we have important titles – but because we have a union sustained and supported by our members. In that sense all our members are present today at the bargaining table today. Every round of negotiations takes place in the context of the times. Three years ago, we negotiated in the shadow of the pandemic. During that time, postal workers courageously stepped up to the challenge as front-line essential workers and, under severe stress, carried out our invaluable mission to the people with great dedication – at a time when the people needed us the most. Our dedication to the postal mission carries on day in and day out, whether in times of pandemics and natural disasters or more “normal” times, and postal workers have earned, and deserve, a good and improved union contract. Today, we are negotiating against a backdrop of both high inflation, with its profound negative impact on workers and our families, along with rising worker militancy throughout the country. Delivery, warehouse, auto, railroad, retail, hotel, manufacturing, grocery, healthcare and education workers have been rising up demanding more of their fair share from employers, all while galloping income inequality enriches the billionaire class. They are fighting, and often striking, to win substantial gains to overcome years of concessionary contracts and falling behind financially. Many of these battles have been focused on ending divisive two-tier wage and benefit systems and getting ahead of the rising cost of food, fuel and housing. In the 2010 collective bargaining agreement, the APWU and the USPS voluntarily reached a deeply concessionary contract for postal workers. Now any objective observer would see these significant concessions as a failure, for both the workers and the wellbeing of the Postal Service. The two-tier wage system which has many workers doing the same work but at significantly lower pay scales causes division, low morale and discriminates against newer and younger workers. Lower wage structures, including the non-career workforce, make it harder for the Postal Service to hire and retain needed positions, and undermines the stability of the workforce, once a mainstay of the Postal Service. There is a direct connection between these problems and the disturbing and deepening delays in mail service. We welcome the progress we have made in the last three rounds of bargaining in overcoming some of the deep concessions from the 2010 contract, including bridging some of the gaps in the tiered wage structure, a better path to career for non-career workers and creating an all-career workforce in the Maintenance Craft and essentially in Motor Vehicle Service craft. But there is more work to do. Obviously, this opening session is not the time to get into specific proposals we will make regarding the issues most important to the postal workers we represent. The “Main Table” will begin meeting today to begin that process. However, generally speaking, the APWU has clear and transparent goals: As postal workers pour our lifeblood into the institution and its mission, workers deserve good annual pay increases, stronger safety rights, an end to the unfair and divisive two-tier career pay scales, limits on subcontracting, a career workforce, and better work hour guarantees and rights for Part Time Flexibles. We advocate that all bargaining unit work in retail be returned to the Clerk Craft and that all the work bargained for in “Jobs Memos” of 2010 finally be returned to the workers as promised. In the light of the impact of profound and rapid technological changes on our jobs, it is high time for a shorter workweek with no loss of pay. And of course, the union strives to protect the hard-won gains and job security provisions secured over generations and for dignity and respect on the job. We will be putting forth proposals to address these and many other issues and concerns. While negotiations will undoubtedly be difficult and at times contentious, let me share a few examples where there should be much common ground: A toxic work environment permeates too many facilities - a long-standing problem in the culture of postal management that cries out for solutions. In good faith we negotiated the “Work Environment Task Force” Memo to address this issue, but it has proven to be a failure. It takes two to tango -- and the management side never looked at the task force as an opportunity to make needed change. Much of the answer depends on the highest levels of management holding managers fully accountable for abuse, whether it is sexual harassment, threats, or bullying, Management should desire to address the endless stream of grievances resulting from constant violations of the union contract. Repeat violators must be held accountable for their flagrant violations and the substantial and unnecessary costs they inflict on the Postal Service, as well as the hardship and anxiety visited upon our members. In addition, management should promote full compliance when issues are settled, whether at Step 1 of the grievance process or arbitration. Continuing battles over settled matters undermine the very intent of our contract to resolve issues at the lowest possible level and that settlements are finding and binding. Those who refuse to comply should no longer be in positions of authority. The union is deeply disturbed by the declining service to the postal patrons. Management ought to share that concern and should be open to considering the union’s proposals to fix the service problems, including the need for proper staffing. Declining service jeopardizes our bond with the people of the country, drives away needed revenue and opens the gates for those who want to privatize the Postal Service. These are just some examples of where the parties, with common ground, should work to resolve problems. The APWU approaches these negotiations as an opportunity to promote our vision for a vibrant public Postal Service and expanded postal services for the people of the country. Our members and our union are passionate about the crucial mission of the public Postal Service, as outlined in the 1970 Postal Reorganization Act: “To provide postal services to bind the Nation together,” to “provide prompt, reliable, and efficient services to patrons in all areas,” and to “render postal services to all communities.” This mission remains in jeopardy, by those on Wall Street who would like to get their hands on the Postal Service’s $78 billion plus in annual revenue, and by ideologues who oppose the very concept of the public good. Yes, we have welcomed opportunities of cooperation with Postmaster General DeJoy as we sought and secured vital postal reform legislation, to expand postal services, return of subcontracted work and in addressing short staffing in mail processing. Yet, there are far too many management practices, some inherited, which have led to severely degraded services, delayed mail, the driving away of customers and revenue. Moving the goalposts on service standards, long-distance consolidation of mail processing and the implementation of network changes are causing havoc and failing to meet the needs of the postal public In addition to some of the general goals I have outlined, the APWU will put forth proposals for improving and expanding financial and other services, from improving certain delivery standards, reactivating Express Mail Services, expanding the network and hours of service, proper staffing, keeping local mail local. We are keenly aware that the Postal Service is still facing serious challenges, including the impact of technology and the internet on the communication habits of the people of the country and the profound and permanent changes to the mail mix - letters are down while packages are up. Such changes create both hardships and hope. While we recognize some of the financial challenges, the finances of the USPS are no longer weighed down by the draconian prefunding mandate from 2006, now eliminated by the 2022 PSRA. In addition, some PRC relief on the price cap has uplifted the finances and the soon to be implemented “Medicare integration” will help the “bottom line” of both employees and the USPS. Management should never forget APWU-represented postal workers voluntarily agreed to over $4 billion of deep wage and benefit concessions in the 2010-2015 contract, resulting in significant and ongoing cost reductions for the Postal Service that carry forward to this day, As we look to the future there are competing visions for the Postal Service. One professes that, in the day of the internet, the Postal Service is a relic of the past. Those who want to destroy us, often funded by the likes of UPS, use these changes to advocate for the breaking up and privatizing of the Postal Service, as did the previous White House administration. Postal workers’ and the APWU’s vision are for a robust and vibrant postal service for generations to come. Those in postal management who believe in the public Postal Service, and I know many of you do, should not be afraid of creative thinking and bold action as we discuss various ways to enhance and expand postal services, rather than play into the hands of those who would like to destroy us on the altar of private profit. This is the fourth round of bargaining in which I am privileged to be the union’s lead negotiator. Each time I have been reminded that former PMG Donohoe shamefully advocated that young workers don’t deserve traditional defined-benefit retirement plans, job security and stable employment and called on Congress to use the Postal Service as “an incubator” for destroying decent jobs. These harmful views found their way into the December 2018 White House “Postal Task Force” recommendations. And much of this thinking led to the formation of the non-career workforce. We vehemently oppose this “race to the bottom.” We believe that the Postal Service should indeed be an incubator, but as it has been for decades, an incubator of good, living-wage union jobs for workers from all walks of life, with equal pay for equal work for women and minorities and solid job opportunities for veterans and an incubator of great public service to every community including new and expanded services for the people of the country. The key to the Postal Service’s successful and bright future remains the hard work and dedication of hundreds of thousands of postal workers – from those who sell postage and accept packages, to those who sort medicine and catalogues, to those who transport the mail and repair the vehicles, to those who maintain the equipment and facilities, to those who deliver the mail. These negotiations are an opportunity for management to reward our dedication and hard work. We recognize and appreciate that in the 2021 round of bargaining, management approached the negotiations in good faith, as did the APWU. The bargaining was hard, but we reached a fair, voluntary agreement, without concessions, that reflected those good faith efforts. We certainly hope that management will approach this round of bargaining with the same spirit. For our part, we will approach these negotiations with a passion for the workers we represent and the public we serve. We will forthrightly share our proposals and be honest in our dealings. We will work hard to achieve a negotiated collective bargaining agreement, subject to approval by our Rank & File Bargaining Advisory Committee and the ratification of our members. We enter these negotiations as part of a movement of friends and allies to protect and enhance a vital and wonderful national treasure that remains a cornerstone in every community. As we meet here on opening day, thousands of APWU members around the country are taking up our mantra, “Good Contract Now! Union Proud, Say It Loud!” as we work to advance the well-being of current and future postal workers, our families and our communities. The APWU is ready to get to work!
-
The LifeBalance Program's 2024 Summer Guide All APWU members and their families have free access to the LifeBalance Program courtesy of the Voluntary Benefits Plan! Sunshine, warm weather, and exciting adventures are on the horizon! Whether you're looking for great deals on attraction admission, rental cars, hotel stays, kids' activities, camping gear, or warm-weather apparel, the LifeBalance Program's 2024 Summer Guide has you covered. Check out the featured deals below, and explore the guide for more! Explore the Guide Universal Orlando Resort Play 4 Days from $65.50 Per Day at Universal Orlando Resort. Priceline Save up to 60% on hotel stays across the US and around the world. Cabela's Stock up on camping and fishing gear, coolers, chairs, outdoor apparel, and more. Save up to $45. Oakley Look sharp and see sharper with Oakley's Prizm polarized lenses. The perfect companion for fun in the sun. Save 15%. Enterprise Need wheels for your summer adventures? From full-size SUVs to sports cars to compact cruisers, get exclusive pricing on rentals. MEL Science Spark a love for science in your kids with monthly hands‑on kits and educational digital experiences. Get 60% off for your first month. View More Deals
-
Melissa Ludwig joined the community
-
With the Postal Service’s restructuring plan moving forward, it is inevitable that Article 12 proposed notices of excessing will appear and may affect multiple occupational groups, ranging from Electronic Technicians, Mail Processing Equipment Mechanics, Maintenance Mechanics, Maintenance Support Clerks, etc. The unfortunate reality is that the Postal Service plans to involuntarily reassign some employees outside of their craft and/ or installation. Below are a few of the required steps that our contract requires prior to excessing: Area/Regional Notification The union at the area/regional level will be given notice when technological, mechanization, or operational changes impact the bargaining unit no less than 90 days in advance, and six months in advance whenever possible. This notice shall be in the form of an Impact/Work Hour Report. Involuntary reassignment of bargaining unit employees outside their craft or installation requires an area/ regional labor-management meeting. It is in the interest of both parties to meet as soon as practicable and to develop an ongoing flow of communications to ensure that the principles of Article 12 (reassignment) are met. The first area/regional labor-management meeting must be held no less than 90 days prior to the involuntary reassignment. Maintenance Craft Discussions Per Article 38.3.K (Excessing) Field managers and/or supervisors should not discuss with bargaining unit employees proposed excessing outside the craft or installation until the area/regional parties have held their discussions. This should prevent employees from receiving erroneous information from management or the union and control the appropriate flow of information. If your office receives an Article 12 proposed notification, you must be ready to challenge the validity of the new Staffing Package by requesting supporting data, emails, rationale, submitted packages, denied submitted packages, approved packages, etc. If you need any help, do not hesitate to contact your Maintenance National Business Agent and Coordinator. We are all working together. The Maintenance Division is offering the workshops below at the National Convention in July 2024. Maintenance Article 12 Excessing Guide Workshop: Addresses how to challenge Maintenance Article 12 Excessing Notifications; Understanding Article 12.5.C.4 and 12.5.C.5, which outlines reassignment within and outside of the Installation, and the applicable Requests for Information (RFIs). (2:30 p.m.-5:30 p.m.) This workshop will be led by NBA Hector Baez. Preserving Maintenance Jobs! In this environment of the Postal Service continuing to revert, or fail to fill, vacant duty assignments, this class will provide a comprehensive look at fighting job reversions, proper remedy requests, and what information to request. This class will also cover sub-contracting of custodial MOU guidelines and the Two-Hour Memo. (10a.m.- 1 p.m.) This workshop will be led by NBA Dave Sarnacki. 2024 Maintenance Negotiation Team: The preparations for national collective bargaining began in January 2024. I am proud to announce the members of our Maintenance Negotiation Team: Idowu Balogun, Maintenance Division Director Terry B. Martinez, Assistant Director A, Maintenance Division Jason Treier, Assistant Director B, Maintenance Division Curtis Walker, National Business Agent, Central Region Dave Sarnacki, National Business Agent, Northeast Region Hector Baez, National Business Agent, Western Region I am honored to select Brother Dana Coletti, president of the Manchester Area Local, as a representative of the Maintenance Division on the Rank-and-File Committee. We welcome your suggestions and comments for the upcoming negotiations. You can contact our team via email Maint2024@apwu.org.
-
https://wvmetronews.com/2024/05/19/postmaster-halts-changes-to-usps-facilities-including-charleston-center-till-next-year/?fbclid=IwZXh0bgNhZW0CMTEAAR1g20JgIZ0eGk6h1FmZpMpjad9RVzN2OG5F7EDWWwIC6YzUKMmCzq7nq6Y_aem_ARpy0DB8d-RIsovHQwpcjdWNwALNw70JuBWfuz_JLplbO5T65qNlUYG4nsTmScvSOPDU9xo4yekCJWaahn1ZidLd
-
June 22nd 6:00AM - 7:00PM @ 711 Bigley Ave, Charleston, WV 25302, the APWU 133 will be hosting an indoor/outdoor diner (food will be provided) with activities. We will also be giving away tee shirts and hoodies first come first serve on certain sizes. We have a pool table, dart board, poker table with playing cards, a large television, and possibly cornhole. We want to encourage all members, family members, and honorary members to come. If there is a dish you would like to bring feel free.
-
In a Needed Step to Improve Service, Postal Management to Slow Down Consolidations In response to union, community, and political pressure, Postmaster General (PMG) DeJoy, in a letter to Senator Gary Peters (D-MI), has agreed to pause, at least until January 2025, a number of the planned mail consolidations that are part of the “network modernization” changes currently underway. (Read the letter here.) PMG DeJoy’s response was in answer to a letter of concern by a bipartisan group of 26 Senators. (Read the Senators’ letter here.) “From the very beginning of these plans, the APWU leadership has advocated that management needs to slow down to ensure that the rights of the workers are upheld and respected and that planned changes must improve service,” said APWU President Mark Dimondstein. “While we acknowledge the need for change in light of changing technology, changes in the mailing habits of the people, and to the mail mix, the network changes have thus far been implemented in a chaotic and detrimental way. Slowing down the process and commitments to improve service are welcome and needed steps.” The letter also commits to not moving forward with any consolidation plans without advising Congress, as well as to moderate the pace of any planned changes. The APWU has initiated a detailed information request to obtain the full and accurate list of consolidations that will be put on hold as well as any potential impact on excessing of employees from one facility to another. “I commend all throughout our union ranks, our community allies and many friends in Congress who have made and will continue to make their voices heard loud and clear – there must be no short cuts when it comes to service,” shared Dimondstein. The APWU will share more information as it is received from the USPS.
-
Craig brown joined the community
-
HAVE YOU BEEN IMPACTED BY U.S. POSTAL SERVICE DELAYS? Senator Manchin strongly opposes cuts to any USPS services in West Virginia and wants to hear your opinion on this important matter. Please consider taking a quick, anonymous survey to help us understand how future changes would affect you. TAKE THE SURVEY
-
"American Postal Workers Union Local 133 was informed this morning, by local media outlets, the USPS has finalized its plan to transfer outgoing mail processing operations to Pittsburgh, PA and Warrendale PA. While it is to no surprise the regurgitated language specified in this release seems to be positive, postal employees across the United States know otherwise. The 10-year Delivering for America Plan is failing you the customer. Recent OIG reports show Texas, Virginia, Georgia and Missouri are all facing backlogs and delays with transportation and mail processing. These reports show mail sitting in trailers for up to two months and financial costs far exceeding the original operational plan before its change. These reports are far from the promised streamlined processing and delivery you have been promised by the service. We want to let our customers and union members know; President Brown and I will continue fighting this consolidation to the fullest extent our contractual provisions allow. We request that members of the public continue to contact their Senators, Congressmen and Congresswomen in opposition to this now planned change." Tim Holstein Vice President APWU Local 133 Charleston, WV
-
The Collective Bargaining Agreement (CBA or union contract) between the APWU and the USPS sets the wages, hours, rights, benefits, job security, and working conditions of APWU-represented postal workers. The current contract expires on Sept. 20, 2024, and preparations are already underway with the official negotiation period beginning this June. The APWU national negotiating team is guided by formal resolutions that are passed by various local and state organizations, and are debated and voted on at our national conventions. We encourage you to work with your local or state union leadership regarding this formal resolution process. However, we also want to hear from each and every one of you. APWU has opened our contract survey so that you can let us know what your priorities are for a new union contract. Please fill out the survey by visiting apwu.org/survey. Alternatively, you can text the word “SURVEY” to 91990 to receive a link to participate in the survey on a mobile device. Contract negotiations are challenging, as management always tries to chip away at our rights, wages, and benefits. Our union is always pushing forward to improve the well-being and job security of postal workers across the country. Please take five minutes to complete the survey and help the APWU negotiate the best contract that we can in 2024! https://www.surveymonkey.com/r/Q5YKS6H
-
March 2024 NPC Report Industrial Relations.pdf
-
James R Berry Jr joined the community
-
IPS Temp Admin joined the community
-
Chad Walker joined the community
-
Brandonray joined the community
-
In accordance with the 2021-2024 Collective Bargaining Agreement, career employees represented by the APWU will receive a $0.17 per hour cost-of-living adjustment (COLA), effective March 9, 2024. The increase is the result of a rise in the Consumer Price Index (CPI-W), and will appear in paychecks dated March 29, 2024 (Pay Period 07-2024). The COLA for full-time employees in each step and grade will amount to $354.00 annually, and the hourly rates for part-time employees will be adjusted accordingly. COLAs are separate and in addition to general wage increases. This is the fifth cost-of-living increase under the 2021 contract. The first increase, effective in February 2022, amounted to $0.63 per hour or $1,310.00 annually. The second, effective in August 2022 was $1.18 per hour or $2,455.00 annually. The third, effective in March 2023, was $0.10 per hour, or $208.00 annually. The fourth, effective August 26, 2023, was 0.48 per hour, or $998.00 annually. The total cumulative COLAs received so far during the 2021-2024 National Agreement is $2.56 per hour, or $5,325.00 annually. Though Postal Support Employees (PSEs) do not receive cost-of-living increases, they have received several additional increases beyond the general wage increases for all employees in the APWU bargaining unit under the 2021 contract. However, when PSEs convert to career, the COLA increases are also included in their base wages going forward. Rising inflation underscores the importance of our negotiated Cost-of-Living Adjustments (COLAs) within our union contract, made possible by the strength of our membership. COLAs are our best protection against inflation. Postal Workers are some of the few U.S. workers who receive COLA increases. Even in the postal world, we are the only postal union that has maintained full COLA in our union contract. “Once again, union-won COLAs prove how invaluable our contractual rights are to postal workers and our families,” said APWU President Mark Dimondstein. “We will continue to fight to maintain full COLA provisions in our upcoming contract.” We will update this article with pay chart information as it becomes available.
-
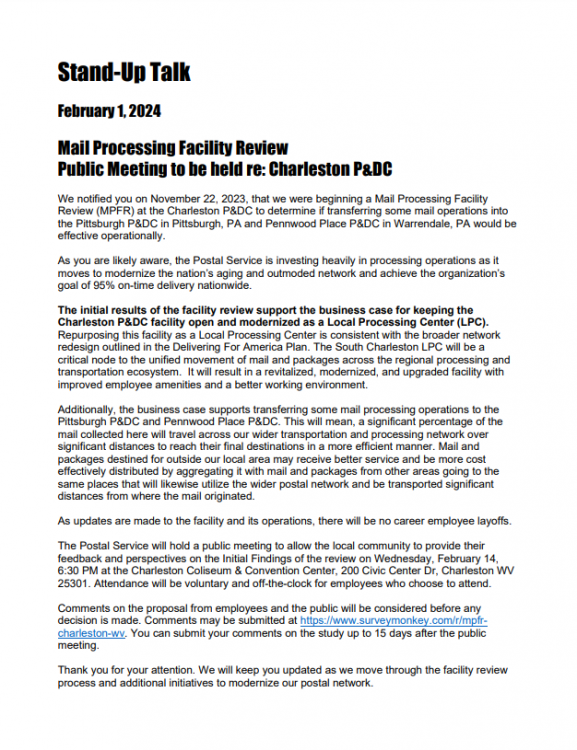
“The Postal Service recently decided to change the Public Meeting date to February 14, at 6:30 pm at the Charleston Civic Center. APWU Local 133 has been inundated with support from local businesses and customers. We have received numerous calls with questions asking why the Postal Service chose this day, when Feb 12 and 13 were available to have the meeting in the same location. The only answer we have is THEY DONT WANT YOU THERE! The union has said from the very beginning, the publics voice is strong, and the postal service does not want to hear it! Please join us at the informational picket at 5pm Tuesday Feb 13 at the Charleston Main Post Office and AGAIN on Valentines Day at the public meeting! We will have over $500 in gift cards to give out in a drawing for all that sign up and attend the meeting. Please feel free to share the above flyer with as many people as you can, and once again, Thank You for helping us fight to keep YOUR mail in West Virginia!” Tim Holstein Vice President APWU Local 133 Charleston, WV
-
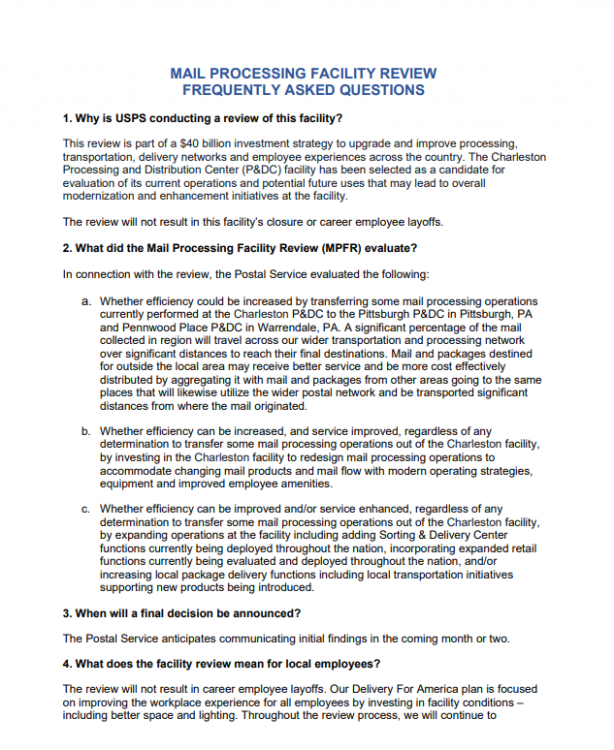
Initial Findings Document Mail Processing Facility Review Charleston P&DC in South Charleston, WV 1/30/2024 As part of a $40 billion investment strategy to upgrade and improve the Postal processing, transportation, and delivery networks, the U.S. Postal Service announced that it is conducting an evaluation of current operations and potential future uses of its Charleston Processing and Distribution Center (P&DC) facility in South Charleston, WV. The USPS ten-year Delivering for America (DFA) plan includes initiatives to improve organizational and operational processes and actively make the Postal Service an efficient, high-performing, world class logistics and delivery provider. Improvements to Postal operations will enhance the level of service provided to the public; drive innovation and enable a broader array of postal products and services; enhance organizational competitiveness; improve efficiency and lower the cost to operate; and provide better workplaces and careers for Postal Service employees. This specific facility review will inform the best allocation of resources and strategies to improve customer service and to achieve significant cost savings through operational precision and efficiency. Business mail entry, Post Office, station, and branch retail services are not expected to change, and delivery services will be unaffected throughout this review. The evaluation is a first step in the Postal Service review and investment process in this facility and will not result in this facility’s closure or career employee layoffs. This ongoing review was initiated to evaluate what role the facility will take in the redesigned postal network and to assess potentially moving some of the mail processing operations from the Charleston P&DC to the Pittsburgh P&DC in Pittsburgh, PA and Pennwood Place P&DC in Warrendale, PA. Below are initial findings from the study: Facility Future The initial results of the facility review support the business case for keeping the Charleston P&DC open and modernizing the facility as a Local Processing Center (LPC) with simplified processes and standardized layouts. The South Charleston LPC will be a critical node to the unified movement of mail and packages across the regional processing and transportation ecosystem in a logically sequenced manner and will benefit from the expanding services the Postal Service plans to deploy to increase its revenue and enhance its role in this community. The facility will offer expanded and streamlined package processing and distribution capabilities in the local market and new workplace amenities for USPS employees. It is anticipated that the facility will maintain the following destinating operations once converted to the LPC: · Destinating Packages · Destinating Letters and Flats · Manual Letters and Flats · Express · Business Mail Entry Unit (BMEU) The LPC will also be fitted with state-of-the-art sorting equipment that will improve delivery services. We plan to operate the following sorting equipment in this facility: · 10 Delivery Bar Code Sorter (DBCS) · 2 DBCS Input Output Subsystem (DIOSS) · 1 Automated Flat Sorting Machine 100 (AFSM 100) · 1 High Speed Tray Sorter (HSTS) · 1 Low-Cost Reject Encoding Machine (LCREM) · 1 Single Induction Package Sorter (SIPS) · 1 Flex Rover Sorter (FRS) The improvements for this facility will result in up to $11 million in investments for modernization efforts and deferred maintenance investments. On the workroom floor, lighting will be upgraded with LEDs, flooring will be repaired and refinished, impediments to open process flow will be removed, and dock areas will be generally rehabilitated. Employee amenities will be refreshed with renovation to restrooms, lockers, and break areas. Parking lots will be repaired and renovated in preparation of both Next Generation Delivery Vehicles (NGDVs), as well as Battery Electric Vehicles (BEVs). Where BEVs will be deployed, we will be upgrading and developing the electrical infrastructure necessary to power the rollout of BEVs into our delivery fleet. New mail and processing equipment investments totaling $7M: · 1 Flex Rover Sorter (FRS) · 1 High Speed Tray Sorter (HSTS) · 1 Single Induction Package Sorter (SIPS) Additionally, the business case supports transferring mail processing outgoing operations to the Pittsburgh P&DC and Pennwood Place P&DC. Currently, a majority of mail and packages are destined outside of the Charleston area to the rest of the world. Finally, the consolidation of plant operations will allow the South Charleston LPC to be collocated with a Sorting and Delivery Center (S&DC). These new facilities are comprised of repurposed facilities and will provide faster and more reliable mail and package delivery over a greater geographic area. S&DCs will be fitted with new package sorting equipment and enable customer service and local commerce opportunities for Same Day or Next Day delivery. They will also have renovated bathrooms and breakrooms for Postal Service employees. In addition, S&DCs will have the infrastructure needed to support the deployment of the Postal Service’s new electric delivery trucks and the charging stations needed to power them. Replacing the Postal Service’s more than thirty-year-old vehicles will allow the organization to significantly reduce carbon emissions, increase safety and reliability, and provide more comfortable delivery vehicles to letter carriers. The S&DC that will be collocated with the South Charleston LPC will have 138 delivery routes that are eligible to be serviced by BEVs. Based on the average deployment numbers at S&DCs, new vehicle investment in BEVs and infrastructure is approximately $5M per site. The Postal Service plans to invest between $20M and $30M into the South Charleston LPC as we prepare the facility to serve as an important contributor to operations in today’s economy and far into the future. Postal Employees NOTE: There will be no career employee layoffs as part of this initiative. The numbers presented here reflect data available as of October 6, 2023, and are subject to change until the completion of the facility review. Our ongoing analysis will include quantifying the time it will take to refurbish the facility and prepare it for the services and functions as an LPC and quantifying the appropriate workforce necessary to efficiently staff the LPC. We expect that the increase in these services and functions may require additional employment positions which could mitigate some of the reductions identified below. Due to the transfer of outgoing operations, an estimated net decrease of 24 craft and 1 management positions are projected once the initiative is completed. All bargaining employee reassignments will be made in accordance with the respective collective bargaining agreements. The Postal Service has made a commitment to ensuring there is a clear path for our pre career employees to obtain fulltime positions, as evidenced by our newly negotiated contract provisions and making automatic conversions to stabilize our workforce. This has culminated in 165,798 pre career employees being converted to career over the past three years. Our pre career workforce is a valuable employee category that provides us necessary operational flexibility leading to efficiencies. Like all employers who have a flexible employee category, there is a higher turnover rate with these employees, providing us the opportunity to both capture savings by rightsizing our workforce when making long overdue operational changes and avoiding any career layoffs. Estimated Cost Savings Proposed savings in the draft MPFR analysis are ultimately projected to be $6.5M - $8.9M annually once the initiative is completed. Below is a breakdown of this savings estimate: · Annual Transportation Savings $4.9M - $6.6M · Annual Maintenance Savings $1.0M - $1.4M · Annual Mail Processing Savings $590K - $790K · Annual Management Savings $90K - $120K Local Customer Considerations · Retail and other services currently available will not change · Business mail acceptance will remain the same · A local postmark will continue to be available at retail post offices · Delivery times of mail to residences and businesses should not change because of the review Commercial Mailers · Mailers who presort mail will continue to receive appropriate postage discounts · Mailers who drop ship to a Destination Sectional Center Facility (DSCF) can expect no changes, if the MPFR is approved Please go to https://www.surveymonkey.com/r/mpfr-charleston-wv to submit written comments. All written comments must be received by February 29, 2024.